Table of Contents
Key Takeaways
- Peptide therapies offer targeted treatment with minimal side effects, making them valuable in primary care.
- Understanding peptide function enhances patient outcomes and supports preventive healthcare strategies.
- Implementing peptides involves comprehensive patient assessment, ongoing education, and strict adherence to regulatory guidance.
- Despite challenges such as cost and regulation, ongoing research suggests a growing and personalized role for peptides in medicine.
Understanding Peptides and Their Role in the Body
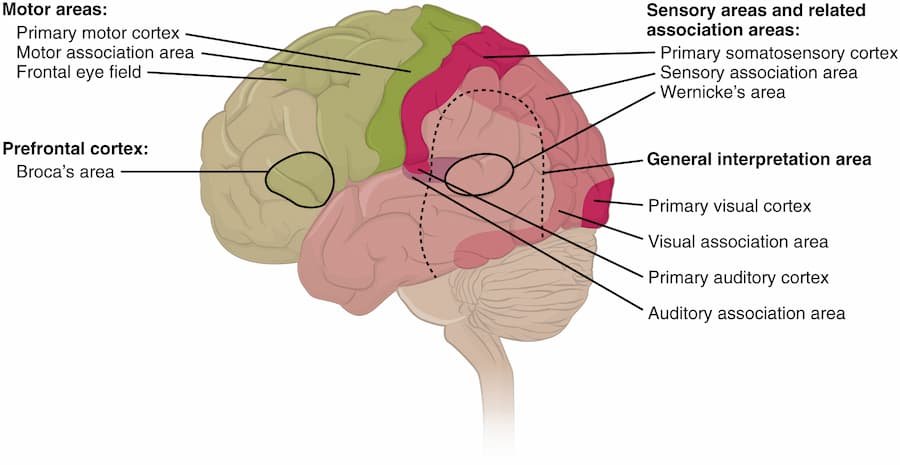
Peptides are biologically active chains of amino acids that act as messengers, regulating critical physiological functions. From modulating hormone levels and metabolic activity to supporting immune responses and healing, their natural compatibility with the human body underpins their growing importance in modern medicine. The potential to fine-tune these powerful molecules makes them highly attractive in primary care settings, where holistic patient management and the prevention of chronic diseases are key priorities.
Clinical research continues to reveal the extensive range of cellular processes influenced by peptides. Their ability to trigger targeted changes at a molecular level means treatments are often more focused, effective, and associated with fewer adverse effects than traditional medications. For patients and practitioners aiming for more precise healthcare approaches, peptides can be seamlessly integrated into wellness, rehabilitation, and disease management protocols.
Advantages of Incorporating Peptides into Primary Care
Peptide therapies offer significant benefits in medical practice by targeting specific biological pathways, which reduces side effects and enhances treatment safety and effectiveness. This precision results in better patient outcomes, improved quality of life, and effective long-term disease management. Patients often experience fewer side effects and quicker benefits, improving treatment adherence. Peptides are versatile, useful as adjuncts for chronic diseases, standalone hormone treatments, or preventive care, making them key tools in personalized and preventive healthcare.
For practitioners interested in exploring the full spectrum of available peptides, comprehensive education and evidence-based practice are key to maximizing therapeutic potential while maintaining patient safety. Continued research and clinical experience will further refine peptide applications, ensuring they remain at the forefront of innovative medical treatments. As awareness grows, both patients and providers stand to benefit from the personalized and targeted approach that peptide therapies uniquely offer.
Common Peptides Used in Primary Care
- Insulin: One of the earliest therapeutic peptides, insulin remains crucial for blood sugar management in the treatment of diabetes. It exemplifies the transformative impact of peptides on the survival of chronic diseases.
- Glucagon-Like Peptide-1 (GLP-1) Agonists: Prescription of GLP-1 agonists has surged due to their efficacy in treating type 2 diabetes and obesity, offering improved glycemic control and additional benefits in weight management.
- Thymosin Alpha-1: This peptide is recognized for its ability to bolster immune defenses and is frequently incorporated for patients facing chronic infections or immune dysfunctions.
- Growth Hormone Releasing Peptides (GHRPs): Used in specific cases for growth hormone deficiencies, muscle wasting disorders, or recovery from injury, illustrating the expanding role of peptide-based solutions.
For more detailed insights into how peptides, such as insulin, function in the body and their therapeutic potential, resources like Medical News Today provide comprehensive overviews. As research progresses, the development of novel peptides promises to enhance patient outcomes further. Continued innovation in this field is likely to significantly expand the range of treatable conditions.
Implementing Peptide Therapy in Clinical Practice
- Education: Staying up-to-date with peer-reviewed data and clinical guidelines ensures the safe and responsible use of peptide therapies.
- Patient Assessment: Individualized evaluation, considering medical history, concurrent treatments, and specific health goals, determines candidacy for peptide integration.
- Monitoring: Regular assessment of outcomes, side effect profiles, and laboratory parameters enables necessary dosage adjustments, thereby maximizing both effectiveness and safety.
Safety and Regulatory Considerations
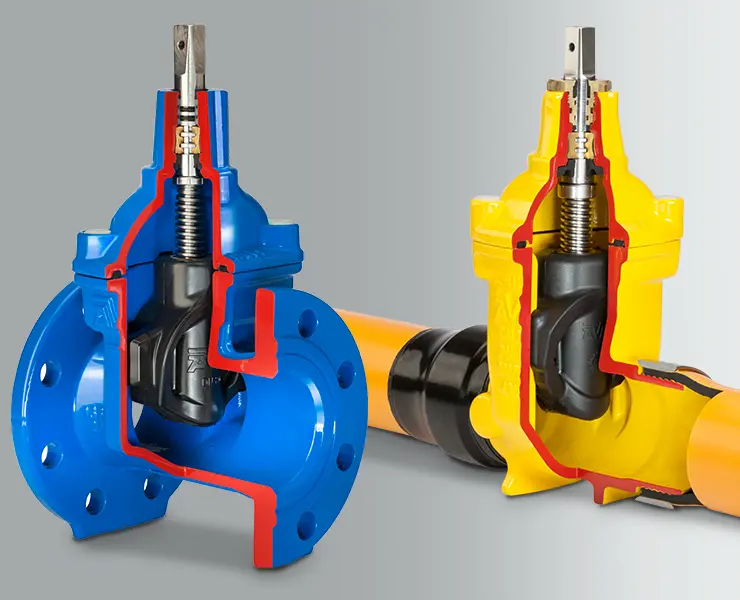
Sourcing peptides from certified, reputable suppliers is crucial to patient safety. Quality assurance helps mitigate the risks of contamination, incorrect formulation, or potency fluctuations. Adherence to local, federal, and international health regulations guides best practices, and periodic review of updated standards is recommended.
Regulatory agencies such as the U.S. Food and Drug Administration (FDA) provide evolving criteria for the classification, compounding, and use of peptide products. Staying compliant reduces the likelihood of legal or medical issues while ensuring consistent therapeutic efficacy.
Challenges in Peptide Integration
- Cost: High manufacturing expenses can impact patient access, especially when peptide therapies are not widely covered by insurance plans.
- Storage and Stability: Many peptides require refrigeration or specialized storage to maintain their biological function until they are administered.
- Regulatory Hurdles: The evolving landscape of peptide approval and licensing presents challenges for both providers and patients as they navigate new treatment options.
Addressing these barriers requires collaborative advocacy and policy engagement, ensuring that access to promising therapies remains a priority in public health settings.
Future Directions in Peptide Therapy
Peptide therapy represents a dynamic frontier in the pursuit of tailored, patient-centered care. With advances in molecular profiling and biotechnology, next-generation peptides are being engineered for enhanced specificity and broader clinical impact. As the medical community continues to learn from large-scale studies and real-world evidence, personalized peptide regimens are expected to become more prevalent in primary care.




































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































0