As personally satisfying as nursing is for passionate individuals, there are a few drawbacks. There’s no career path easy. Going through challenges and various ups and downs is part of life.
But nursing is a profession that demands the most from healthcare professionals. One common hurdle for nurses is difficult patients.
Hospitals encounter a host of individuals from different walks of life, and once in a while, a hot-headed, irritable, or aggressive patient makes it to the treatment room.
Handling them can be particularly challenging for inexperienced nurses in the industry. Yes, the situation is stressful, and the risk of escalation is significant, but it is never out of your capacity to control.
With the right techniques and appropriate response, even the most aggressive patients can be handled.
However, remember never to compromise your safety and maintain clear boundaries. If you are new to the industry, the following tips will help you cope with almost any situation.
Table of Contents
1. Don’t invade their personal space
Each of us has a different boundary of personal space that we expect others to respect, and anyone who doesn’t comply makes us uncomfortable.
To keep a difficult patient calm, don’t invade their personal space as this threatening gesture can elevate anxiety.
Keep your patients at arm’s length and if you must approach them, give them a reason first. Aggressive patients can lash out if they feel threatened, so respecting personal space helps keep you out of danger.
If you cannot deescalate the situation and the patient is physically abusive, you can always resort to pressing charges against the perpetrator.
Such is also true for the opposite case scenario where patients suffer abuse or neglect at the hands of the healthcare provider and can call in nursing home abuse lawyers, for instance.
Laws exist to protect the rights of both parties and should be used, but only as a last resort.
2. Don’t be defensive
An angry patient’s anger and frustration are not directed at you, and you are not the one to blame. It usually stems from some other experience or the distress of the illness in general.
Don’t let your posture convey that you are on the defensive. Keep your hands open and relaxed in front of your body and maintain eye contact but avoid staring.
The situation is not about you; it is about the patient, so don’t take things personally. Keep your frustrations in check and maintain your cool regardless of whether you are right.
3. Be compassionate
While you must maintain a neutral facial expression, communicate through your words and expressions, implying that you understand the patient and are empathetic towards them.
Doing so conveys a peaceful stance towards them and informs them that they aren’t alone. Phrases like ‘I get that this is difficult on you and your family’ can help.
Use these strategies to establish trust and understanding with the patient.
4. Monitor your body language
Your body language says a lot about your intentions to a patient, and some postures appear threatening to them.
Sometimes, eye-to-eye contact with a toe-to-toe position can be interpreted by the patient as challenging or threatening.
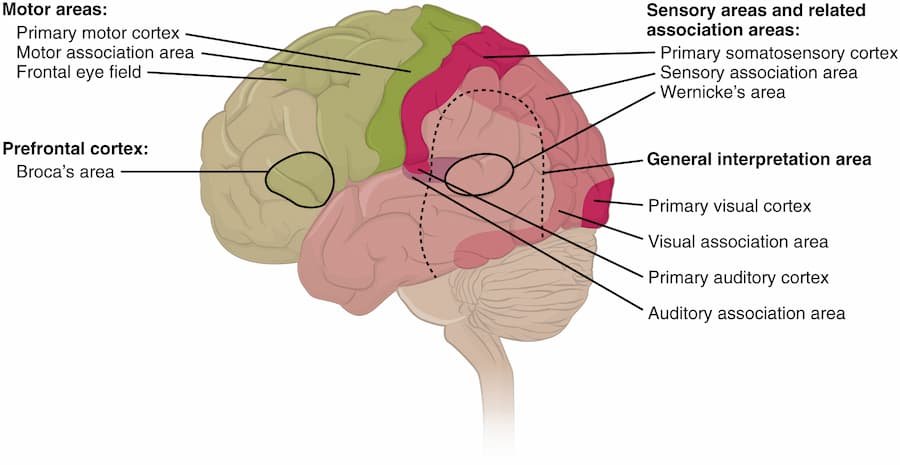
This can induce a fight-or-flight response and result in a negative outcome. It is best to maintain a sideways posture and stand at an angle.
This position is known as the Supportive Stance in CPI training. It is known to minimize the subject’s anxiety, enhance communication, and make the situation non-threatening to them.
5. Let them vent out to you
Sometimes, being accustomed to telling patients what to do, nurses overlook that they aren’t giving the patients time to speak for themselves.
Provide them a listening ear and let them vent out their frustrations. This way, you will understand what is troubling them and what they are feeling.
This stance will help you collaborate with them to address the underlying problem. At the same time, this reduces the chances of things escalating to physical violence as it releases much of their frustration verbally.
6. Listen actively
Active listening is the art of listening while keeping the partner engaged, understanding what they are saying, reflecting on it, and paraphrasing.
Active listening makes sure that the speaker knows that you heard them attentively. You should pay attention, avoid distractions, and let your non-verbal behavior demonstrate this.
Keep a check on your facial expressions and avoid negative reactions. It is best to maintain eye contact 60 to 70% of the time.
It shouldn’t be interpreted as staring as it can get overwhelming and shouldn’t be so infrequent that it appears that you are uninterested.
Once you have attentively heard the patient’s point, reflect on it and summarize what you interpreted from their words; this helps them feel you understood and their emotions are validated.
Also, remember to remain neutral and non-judgmental so that the patient doesn’t feel blamed or criticized. Active listening establishes a positive relationship with the patient.
7. Don’t respond to challenging questions
The patient’s verbally aggressive behavior can inevitably frustrate or irritate you, but remember to keep your response in check.
Do not engage in a power struggle even when the patient challenges your authority or argues against an organizational policy.
For instance, if a patient responds with ‘who are you to tell me to do anything?’ do not entertain the challenge as it will only escalate the situation.
It is best to ignore the challenge and move on calmly and respectfully.
8. Resort to physical restraint only if all else fails
Calling in security should be your last resort and should be avoided if possible. Yes, you do not have to tolerate any physical threat to yourself but remember that physical intervention risks injury to those involved.
Do so only if you believe that not intervening will be more dangerous. Secondly, physical intervention should only be practiced by trained staff members who know which methods are safest and least restrictive.
Defusing an escalating situation is necessary, but it is not always possible to use non-physical means alone. Some regulations exist about physical restraint in healthcare settings.
Final words
Nursing is not as smooth as most might expect. Encounters with difficult and even abusive patients are inevitable, but skilled nurses should know the best ways to deescalate the situation.
When encountering such a situation, remember not to invade the patient’s personal space, keep a non-threatening posture, be compassionate, let the patient vent out, and listen attentively.
Remember, only resort to physical restraint when nothing else works.















































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































0