Table of Contents
A New Obesity Paper Has Diet Researchers Rired Up
A new paper has the obesity treatment community on the edge of its seats. But why? There’s a good reason: The paper’s findings contradict the prevailing wisdom. Although energy can’t be created or destroyed, it certainly must go somewhere if more is consumed than expended. The energy balance theory, however, still doesn’t answer the “why” question.
Energy balance theory
The energy balance theory for obesity explains the interplay between energy intake and expenditure and the level of energy stored in the body. It suggests that in order to prevent obesity, people should modify their energy intake and expenditure, rather than simply restricting calories. According to this model, the primary cause of obesity is overeating, and the main culprit is the overconsumption of energy-dense, inexpensive foods.
The energy balance theory has been widely used in obesity studies. It claims that body weight is stable when average energy intake equals average energy expenditure. However, it is unlikely that a steady state of body weight will occur without a sustained energy imbalance. In fact, mathematical analysis has shown that energy balance is necessary for weight stability to occur. It also argues that a sustained positive energy balance is necessary for a person to lose weight, thereby reducing body fat levels.
Carbohydrate insulin model
David Ludwig has been an energetic advocate of the carbohydrate-insulin model for obesity, and he hopes that it will replace energy balance as the dominant framework for thinking about obesity. However, he’s raised several questions about the validity of this model. The first question, which Ludwig addressed in a recent paper, is whether the double-labeled water method is accurate.
The carbohydrate-insulin model of obesity suggests that diets high in carbohydrates are particularly fattening because they cause elevated levels of insulin, which directs energy toward storage as fat in adipose tissue and away from oxidation in metabolically active tissues. This leads to a perceived state of cellular internal starvation, which induces an increase in hunger and suppressed metabolism, thereby leading to weight gain. However, the evidence supporting the model is not very strong.
Mechanisms of fat storage
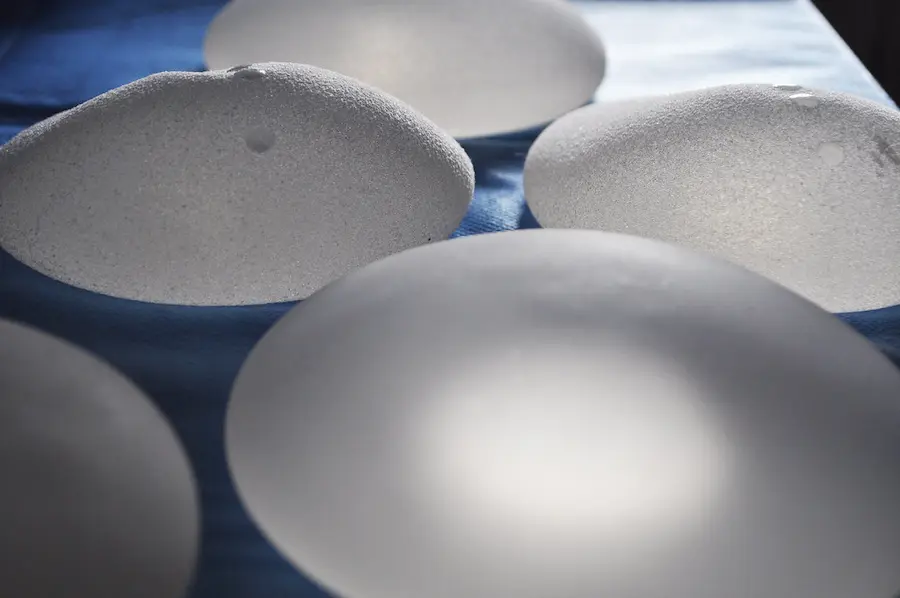
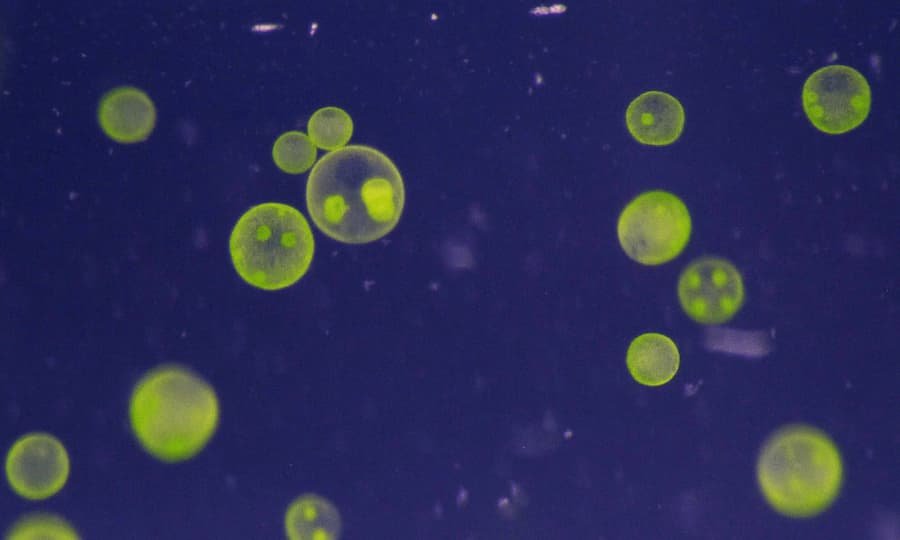
One of the most important questions to ask about obesity is how the body stores excess calories. A classic compartment for storing excess calories is the subcutaneous fat tissue. This tissue acts as an insulator and is a source of energy. However, obesity leads to increased insulin resistance, which increases the risk of diabetes, obesity, and COVID-19 complications. Researchers are currently trying to learn more about this tissue type and the mechanisms that regulate its storage.
The number of fat cells in an individual is related to the amount of fat stored. Adipose tissue stores fatty acids in two ways. The first is by uptake, and the other is through oxidation.
Low-fat diet craze
During the low-fat diet craze, processed carbohydrates flooded the food supply, raising insulin levels and suppressing glucagon levels. This hormonal imbalance directs excess calories toward fat storage and leaves few calories available for metabolically active organs. These changes result in weight gain and obesity.
Several studies have shown that the low-fat diet has no discernible impact on the risk of heart disease. One study, the Women’s Health Initiative, included thousands of women and showed no reduction in cardiovascular disease risk. However, since the study was conducted nearly 40 years ago, many other changes in Americans’ lifestyles have taken place. For example, many people have quit smoking, exercised more, and started taking statins. This has made it more difficult to detect a diet-related effect on the risk of heart disease.
Overeating
Overeating and obesity are connected to a wide range of factors, from eating habits to physical activity and sleep patterns. Whether it’s habitual or the result of stress, the act of overeating causes the body to store excess calories as fat. As a result, obesity and overweight increase the risk of developing chronic health conditions. Overeating also affects the body’s digestion. Because of this, it may take longer for food to be broken down, which ultimately means more fat is stored.
Studies have suggested that overeating may contribute to poor sleep. The circadian clock is responsible for controlling sleep, and eating too much disturbs this rhythm. Fortunately, overeating can be prevented by eating sensibly and paying attention to portion sizes. Instead of snacking on highly processed foods, eat fresh fruits and vegetables. These contain fiber and can reduce the tendency to snack on unhealthy foods. Using a salad plate can also help control portion sizes.
Insufficient physical activity
A recent study on the obesity pandemic has roiled health and science circles. The paper by Harvard University professor David S Ludwig challenges a widely held view that weight gain is primarily a result of a lack of physical activity. The study challenges the “energy balance model” that suggests eating less and doing more physical activity. The model has long been promoted by governments and health organisations. The USDA Dietary Guidelines for Americans recommend reducing calorie intake while increasing physical activity.
The study used data from the National Health and Nutrition Examination Survey, a long-term project of the Centers for Disease Control and Prevention. The survey included results from 17,430 participants from 1988 to 1994 and another five thousand participants a year from 1995 to 2010. Each survey participant recorded the amount, frequency, and intensity of physical activity in the previous month. The researchers defined ideal exercise as at least 150 minutes of moderate physical activity a week and 75 minutes of vigorous exercise.



































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































































0